July 26, 2025
This comprehensive guide aims to provide tips and tricks of interpreting LF pMRI, specifically the Hyperfine Swoop® MRI system, which operates at 0.064 T and is currently the only FDA and Health Canada approved LF pMRI system.
Purpose of the Guide
This paper offers a thorough overview of the operational nuances and interpretive complexities unique to LF pMRI, emphasizing the importance of proper patient positioning, tailored protocol selection, and awareness of imaging artifacts that may arise. It also addresses the common diagnostic challenges associated with low-field imaging and provides illustrative examples to support clinical integration. The ultimate aim is to equip current and prospective users with practical strategies to maximize image quality, ensure accurate interpretation, and navigate common pitfalls with confidence.
How the Guide Was Done
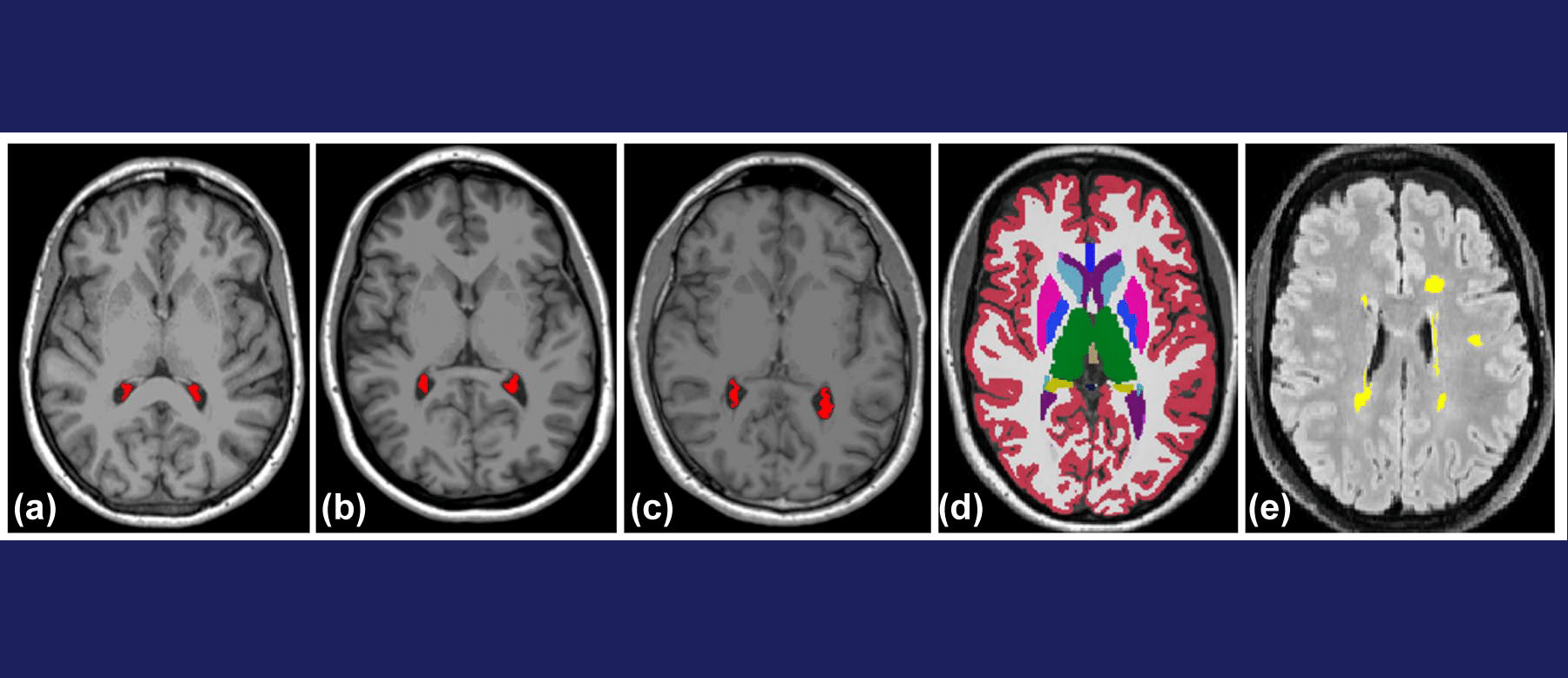
Our institution has scanned over 250 patients since implementation in March 2022. Imaging sequences that are currently available on the Hyperfine Swoop® MRI system include 3D anisotropic T1-weighted (inversion prepared fast-spin-echo (FSE)), T2-weighted (FSE), FLAIR (inversion-prepared FSE), and DWI/ADC sequences. There are unique interpretive and physics considerations related to low field magnet design and low frequency radiofrequency (RF) coil architecture, as well as image processing algorithms that reduce noise and improve image quality in the millitesla regime.
Key Findings
Low-field portable MRI (LF pMRI) offers a valuable bedside neuroimaging solution for critically ill or non-transportable patients. While it provides key advantages in accessibility and monitoring morphological brain changes, LF pMRI comes with diagnostic limitations such as reduced sensitivity to hemosiderin and infarcts, limited contrast performance with gadolinium agents, and the need for tailored protocols. Effective implementation requires operational coordination, especially for patient positioning. The publication calls for formal education and collaborative training to help radiologists adopt this modality confidently and integrate it into routine clinical care.
Who Developed the Guide
The guide was conceived by Drs. Amy Chen, Shobhit Mathur, Amy Lin, and Aditya Bharatha.
Link to Publication: